Dual Special Needs Plans (DSNPs) are an important part of providing health coverage to dually eligible Medicare and Medicaid beneficiaries and those who receive varying levels of low income subsidies.
As we enter 2025, it’s critical for insurance agents to stay updated on eligibility requirements, plan definitions, and state-specific rules as the landscape has changed. In 2025 the quarterly LIS and Dual Eligible SEP is being eliminated, and replaced with two new monthly SEPs
- LIS and Dual eligible members can disenroll from their current Medicare Advantage plan and enroll into a standalone PDP with original Medicare. (Plans you can’t sell monthly)
- Full dual eligible members can enroll into an aligned or integrated D-SNP plan IF they are currently enrolled into the Medicaid MCO from the parent company. (Plans you can sell monthly that vary by state, county, and carrier listed below)
This guide summarizes what you need to know as well as provides a direct link to the CMS file where the data referenced below can be accessed. Also important updates, including training mandates, LIS SEP guidelines, Medicaid alignment, and D-SNP eligibility levels are listed below to help you understand what you can and can’t sell monthly outside of AEP when using an LIS SEP.
Table of Contents
- State Training Requirements
- LIS SEP Rules by State
- Medicaid Alignment: Automatic vs. Manual
- Medicaid Eligibility Groups and Income/Asset Limits
- Plan Definitions: HIDE, FIDE, and More
- Key Takeaways for 2025
State Training Requirements
Virginia has implemented mandatory training for agents selling FIDE DSNPs. Agents must complete these trainings to remain compliant:
- Aetna & Molina: Virginia DMAS FIDE training is required and accessible via the DSNP folder in Data Central. Completion certificates must be downloaded for verification.
- UnitedHealthcare: Agents must annually complete a DMAS training video and attest to compliance.
- Elevance: A 20-minute training video titled “Enrolling Beneficiaries into Virginia Dual Eligible Special Needs Plans” is required.
- Other carriers: Carriers are still finalizing their requirements and we will add these as we receive them
Without completing these trainings, agents cannot assist clients with DSNP enrollments in Virginia.
We will continue to update as more states adopt specific training processes.
LIS SEP Rules by Carrier & State
Below is a breakdown of the carriers that you can sell monthly along with each of the states and plans that can be sold as well as additional information for each carrier. If you have a customer that resides in a restricted state, they will have to wait until AEP or OEP to make a plan switch.
2025 HIDE FIDE Plans by State
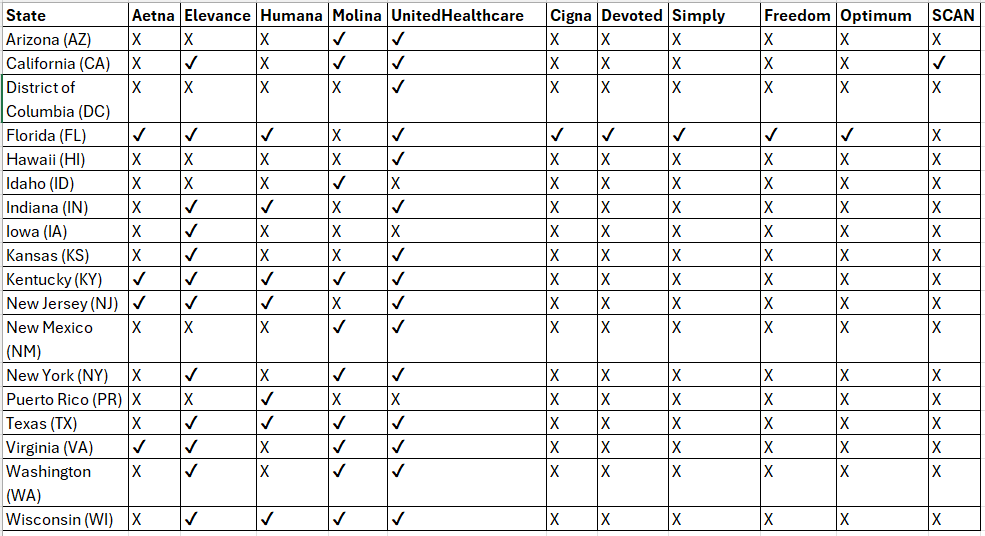
Aetna
- HIDE/FIDE States (Monthly LIS SEP Available): Florida (FL), Kentucky (KY), New Jersey (NJ), Virginia (VA)
- Restricted States (AEP/OEP Only): Alabama (AL), Arkansas (AR), Arizona (AZ), California (CA), Colorado (CO), Connecticut (CT), Delaware (DE), Georgia (GA), Iowa (IA), Illinois (IL), Kansas (KS), Louisiana (LA), Maryland (MD), Maine (ME), Michigan (MI), Missouri (MO), Mississippi (MS), North Carolina (NC), Nebraska (NE), Nevada (NV), New York (NY), Ohio (OH), Oklahoma (OK), Pennsylvania (PA), South Carolina (SC), South Dakota (SD), Texas (TX), Utah (UT), West Virginia (WV)
- Virginia Training Requirement: Agents must complete DMAS FIDE training before selling in Virginia. If completed, agents can download their certificate from the DSNP folder in Data Central.
- States That Automatically Change Medicaid: Florida (FL), New Jersey (NJ), Virginia (VA)
- Medicaid Alignment Requirement: Kentucky (KY)
- HIDE/FIDE Plan Contract Numbers: FL H1609-017, 019, 043, 044, 045, 046, 047, 048, 049, 055, 056, 061, 062, 064, 065; KY H0628-012; NJ H6399-001; VA H1610-001
- County Service Areas: FL 34 counties, KY 71 counties, NJ Statewide, VA Statewide
Elevance
- HIDE/FIDE States (Monthly LIS SEP Available): California (CA), Indiana (IN), Iowa (IA), Kansas (KS), Kentucky (KY), New Jersey (NJ), New York (NY), Tennessee (TN), Texas (TX), Virginia (VA), Washington (WA), Wisconsin (WI)
- Restricted States (AEP/OEP Only): Arizona (AZ), Colorado (CO), Connecticut (CT), Georgia (GA), Louisiana (LA), Maine (ME), Missouri (MO), Nevada (NV), Ohio (OH)
- Virginia Training Requirement: Brokers selling 2025 Dual Eligible Special Needs Plans in Virginia must complete a 20-minute training video titled “Enrolling Beneficiaries into Virginia Dual Eligible Special Needs Plans.”
- States That Automatically Change Medicaid: CA, IN, IA, KS, NJ, NY, TN, TX, VA, WA, WI
- Medicaid Alignment Requirement: Kentucky (KY)
- HIDE/FIDE Plan Contract Numbers: CA H4471-001; IN H3447-048, 055; IA H0907-001, 003; KS H6316-005; KY H9525-007, 019; NJ H3240-013, 024; NY H8432-041, 042; TN H5828-001; TX H2593-044, 045, 046, 047; VA H4694-001, 003, 004; WA H1894-002; WI H9525-003, 018
- County Service Areas: CA (8 counties), IN (Statewide), IA (Statewide), KS (47 counties), KY (Statewide), NJ (21 counties), NY (10 counties), TN (Statewide), TX (132 counties), VA (94 counties), WA (23 counties), WI (Statewide)
Humana
- HIDE/FIDE States (Monthly LIS SEP Available): Florida (FL), Kentucky (KY), Indiana (IN), New Jersey (NJ), Puerto Rico (PR), Wisconsin (WI)
- Restricted States (AEP/OEP Only): Nebraska (NE), Missouri (MO), Texas (TX), Colorado (CO), North Carolina (NC), Mississippi (MS), Louisiana (LA), New York (NY), Georgia (GA), Tennessee (TN), Arkansas (AR), West Virginia (WV), Pennsylvania (PA), Oklahoma (OK), Iowa (IA), South Carolina (SC), Maine (ME), Utah (UT), Nevada (NV), Maryland (MD), Michigan (MI), North Dakota (ND), Ohio (OH), California (CA), Indiana (IN), Alabama (AL), Washington (WA), Montana (MT)
- Virginia Training Requirement: None specified
- States That Automatically Change Medicaid: FL, IN, NJ, PR, WI
- Medicaid Alignment Requirement: Kentucky (KY)
- HIDE/FIDE Plan Contract Numbers: FL H1019-023, 073, 146, 077, 102, 209, 210, 213, 214, 226, 280, 285, 304, 214, 394, 003, 010; IN H5619-054; KY H1036-235, H5525-045, H5619-075, 163, H6622-018; PR H4007-016, 018, 026, 027, 030, 031; WI H2237-001, 007, H5216-420
- County Service Areas: FL (65 counties), KY (120 counties), IN (92 counties), PR (78 counties), WI (30 counties)
Molina
- HIDE/FIDE States (Monthly LIS SEP Available): Arizona (AZ), California (CA), Idaho (ID), Kentucky (KY), Nebraska (NE), New Mexico (NM), New York (NY), Texas (TX), Virginia (VA), Washington (WA), Wisconsin (WI)
- Restricted States (AEP/OEP Only): Michigan (MI), Mississippi (MS), Ohio (OH), South Carolina (SC), Utah (UT)
- Virginia Training Requirement: Agents must complete DMAS FIDE training before selling in Virginia. Completed certificates can be downloaded from the DSNP folder in Data Central.
- States That Automatically Change Medicaid: AZ, CA, ID, KY, MA, NE, NM, NY, TX, VA, WA, WI
- Medicaid Alignment Requirement: Kentucky (KY)
- HIDE/FIDE Plan Contract Numbers: AZ H8845-001; CA H3038-003, H5649-002; ID H5628-008; KY H1799-001, 002, 003; MA H2224-001, 003; NE H2715-005; NM H8845-006; NY H5992-001, 002, 007, 009; TX H7678-001, H2715-002; VA H7559-001; WA H5823-006; WI H5209-002, 004
- County Service Areas: AZ (3 counties), CA (23 counties), ID (34 counties), KY (75 counties), MA (8 counties), NE (56 counties), NM (32 counties), NY (18 counties), TX (87 counties), VA (Statewide), WA (Statewide), WI (44 counties)
UnitedHealthcare
- HIDE/FIDE States (Monthly LIS SEP Available): Arizona (AZ), District of Columbia (DC), Florida (FL), Hawaii (HI), Indiana (IN), Kansas (KS), Kentucky (KY), Nebraska (NE), New Jersey (NJ), New Mexico (NM), New York (NY), Texas (TX), Virginia (VA), Washington (WA), Wisconsin (WI)
- Restricted States (AEP/OEP Only): Alabama (AL), Arkansas (AR), California (CA), Colorado (CO), Connecticut (CT), Delaware (DE), Georgia (GA), Iowa (IA), Idaho (ID), Illinois (IL), Louisiana (LA), Maine (ME), Maryland (MD), Michigan (MI), Minnesota (MN), Missouri (MO), Mississippi (MS), Montana (MT), North Carolina (NC), North Dakota (ND), New Hampshire (NH), Nevada (NV), Ohio (OH), Oklahoma (OK), Oregon (OR), Pennsylvania (PA), Rhode Island (RI), South Carolina (SC), South Dakota (SD), Tennessee (TN), Utah (UT), Vermont (VT), West Virginia (WV), Wyoming (WY)
- Virginia Training Requirement: Virginia agents are required to complete a DMAS video and sign an attestation form before completing a 2025 Virginia D-SNP enrollment. The training is mandatory annually.
- States That Automatically Change Medicaid: AZ, DC, FL, HI, IN, KS, NE, NJ, NM, NY, TX, VA, WA, WI
- Medicaid Alignment Requirement: Kentucky (KY)
- HIDE/FIDE Plan Contract Numbers: AZ H0321-002; DC H2406-053, H7464-010; FL H1045-012, 039, 061, 063, 064, 065, 002, 026, 003, 006, 015, 016; HI H2406-051, 132; IN H2001-064, 067; KS H0169-004, 029; KY H1889-008, 030, H6595-003, 004, 005; NE H0169-003, 006, H2001-054, H2802-053; NJ H3113-005; NM H0294-049, 050; NY H3387-014, 013; TX H4514-021; VA H0421-001, H2445-003, 005; WA H2001-051, 081, H5008-002; WI H0294-027, H3794-002, 004, 006, H5253-024
- County Service Areas: AZ (15 counties), DC (2 counties), FL (51 counties), HI (5 counties), IN (91 counties), KS (43 counties), KY (66 counties), NE (45 counties), NJ (12 counties), NM (21 counties), NY (54 counties), TX (56 counties), VA (83 counties), WA (9 counties), WI (39 counties)
Cigna
- HIDE/FIDE States (Monthly LIS SEP Available): Florida (FL)
- Restricted States (AEP/OEP Only): Alabama (AL), Arkansas (AR), Colorado (CO), Connecticut (CT), Delaware (DE), Georgia (GA), Maryland (MD), Missouri (MO), Mississippi (MS), North Carolina (NC), Ohio (OH), Pennsylvania (PA), Tennessee (TN), Texas (TX)
- Virginia Training Requirement: Not applicable
- States That Automatically Change Medicaid: FL
- Medicaid Alignment Requirement: Not applicable
- HIDE/FIDE Plan Contract Numbers: FL H5410-031, 042, 047, 049
- County Service Areas: FL (32 counties)
Devoted Health
- HIDE/FIDE States (Monthly LIS SEP Available): Florida (FL)
- Restricted States (AEP/OEP Only): Alabama (AL), Arkansas (AR), Arizona (AZ), Colorado (CO), Missouri (MO), Mississippi (MS), Michigan (MI), Ohio (OH), Pennsylvania (PA), Tennessee (TN), Texas (TX)
- Virginia Training Requirement: Not applicable
- States That Automatically Change Medicaid: FL
- Medicaid Alignment Requirement: Not applicable
- HIDE/FIDE Plan Contract Numbers: FL H1290-042, 052, 054
- County Service Areas: FL (27 counties)
Simply Healthcare
- HIDE/FIDE States (Monthly LIS SEP Available): Florida (FL)
- Restricted States (AEP/OEP Only): Not applicable
- Virginia Training Requirement: Not applicable
- States That Automatically Change Medicaid: FL
- Medicaid Alignment Requirement: Not applicable
- HIDE/FIDE Plan Contract Numbers: FL H5471-064, 066, 072, 076, 082, 084, 111, 115, 118, 121, 125
- County Service Areas: FL (14 counties)
Freedom Health
- HIDE/FIDE States (Monthly LIS SEP Available): Florida (FL)
- Restricted States (AEP/OEP Only): Not applicable
- Virginia Training Requirement: Not applicable
- States That Automatically Change Medicaid: FL
- Medicaid Alignment Requirement: Not applicable
- HIDE/FIDE Plan Contract Numbers: FL H5427-087
- County Service Areas: FL (24 counties)
Optimum Healthcare
- HIDE/FIDE States (Monthly LIS SEP Available): Florida (FL)
- Restricted States (AEP/OEP Only): Not applicable
- Virginia Training Requirement: Not applicable
- States That Automatically Change Medicaid: FL
- Medicaid Alignment Requirement: Not applicable
- HIDE/FIDE Plan Contract Numbers: FL H5594-017
- County Service Areas: FL (24 counties)
Medicaid Alignment: Automatic vs. Manual
Some states simplify DSNP enrollments by automatically aligning Medicaid with DSNP plans, while others require manual changes. Key states include:
Automatic Medicaid Alignment:
- Aetna: FL, NJ, VA
- Elevance: AZ, CA, FL, IA, KS, NJ, NY, TN, TX, VA, WA, WI
- Humana: FL, IN, NJ, PR, WI
- Molina: AZ, CA, ID, KY, MA, NE, NM, NY, TX, VA, WA, WI
- UnitedHealthcare: AZ, DC, FL, HI, IN, KS, NE, NJ, NM, NY, TX, VA, WA, WI
Manual Changes Required
Kentucky, agents must assist clients in aligning their Medicaid with DSNPs manually.
Medicaid Eligibility Groups and Income/Asset Limits
D-SNP eligibility is determined by income, assets, and benefit needs. Below is a summary of eligibility groups:
- Qualified Medicare Beneficiaries (QMB):
- Income: $1,275 (Individual), $1,724 (Married Couple)
- Assets: $9,430 (Individual), $14,130 (Married Couple)
- Coverage: Part A & B premiums and cost-sharing (No full Medicaid)
- QMB Plus:
- Income/Assets: Same as QMB
- Coverage: Part A & B premiums, cost-sharing, and full Medicaid benefits
- Specified Low-Income Medicare Beneficiaries (SLMB):
- Income: $1,526 (Individual), $2,064 (Married Couple)
- Coverage: Part B premium only (No Medicaid)
- SLMB Plus:
- Income/Assets: Same as SLMB
- Coverage: Part B premiums, partial cost-sharing (varies by state), and full Medicaid
- Qualified Disabled and Working Individuals (QDWI):
- Income: $5,105 (Individual), $6,899 (Married Couple)
- Assets: $4,000 (Individual), $6,000 (Married Couple)
- Coverage: Part A premium only
- Qualifying Individuals (QI):
- Income: $1,715 (Individual), $2,320 (Married Couple)
- Coverage: Part B premiums only
- Full Benefit Dual Eligible (FBDE):
- Income/Assets: Determined by state
- Coverage: Medicaid and some Medicare benefits
Plan Definitions: HIDE, FIDE, and More
Understanding D-SNP plan structures is key for agents. Here are critical definitions:
Fully Integrated Dual Eligible (FIDE):
- FIDEs are an integrated plan type under a single legal entity that has both a contract with CMS for MA and a contract with the state for Medicaid. The plan is required to have exclusively aligned enrollment meaning that the FIDE plan’s membership is limited to dually eligible beneficiaries who receive their Medicare and Medicaid managed care coverage from plans owned and operated by the same parent company.
- Combines Medicare and Medicaid benefits under a single legal entity.
- Requires coverage of primary, acute, and long-term care services, including 180 days of nursing facility care.
Highly Integrated Dual Eligible (HIDE):
- HIDE plan is a Highly Integrated Dual Eligible Special Needs Plan and unlike the FIDE is not required to have exclusively aligned enrollment in 2025. A HIDE is required to cover EITHER the LTSS benefits OR behavioral health, but is not required to cover both like a FIDE. HIDE’s may also exclude additionally offered Medicaid benefits from their coverage
- Covers Medicaid benefits, LTSS, and behavioral health through capitated contracts.
- HIDE contracts must cover the entire D-SNP service area as of 2025.
Applicable Integrated Plan (AIP):
Includes HIDE or FIDE plans with exclusively aligned enrollment.
Coordination Only (CO) D-SNPs:
Meet CMS requirements but lack HIDE/FIDE integration. CO plans coordinate Medicare and Medicaid services but do not integrate them fully.
Exclusively Aligned Enrollment (EAE):
Limits enrollment to full-benefit dually eligible individuals. EAE plans integrate Medicare and Medicaid services with unified materials and streamlined processes.
Confirming Plan Status
If you would like to download the full CMS landscape file which is the source of this data, you may download the file here. Below are the columns you will need to filter to see the full breakdown of carriers, states, counties, and plans.
- Download the CSV file and Create a filter
- Adjust Column R – Dual Eligible SNP (D-SNP) Integration Status and select HIDE and FIDE.
- Adjust Column S – D-SNP Applicable Integrated Plan (AIP) Identifier and select Yes.
- View all carriers and plans in your market.
Here is a DSNP SEP Guide produced by CMS that has additional information.
2025 LIS SEP Takeaways
- Complete Mandatory Training: Agents selling in Virginia must comply with carrier-specific training requirements.
- Understand State Rules: Review LIS SEP restrictions and Medicaid alignment processes by state.
- Know Eligibility: Familiarize yourself with income/asset limits and benefits for each eligibility group.
- Leverage Plan Options: Understand HIDE, FIDE, and CO structures to guide clients effectively.
- Work with your FMO: Work closely with your FMO to target your core states and figure out what you can and can’t compliantly sell throughout the off season.
By clearly understanding these updates and definitions, you’ll be well-equipped to provide exceptional service to your clients in 2025. Be sure to continue to access training and resources through your carrier portals as well as pay close attention to carrier emails on this topic to stay informed.
For agencies contracted with SMA, please contact your account manager to discuss your specific markets that are impacted by these new rules.


